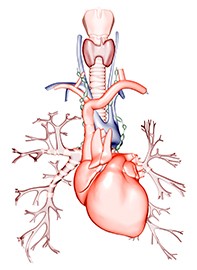
Thyroid disease: how does it affect the heart?
Both hyperthyroidism and hypothyroidism can seriously affect cardiovascular health. This article discusses the mechanisms by which thyroid disease can affect the cardiovascular system, diagnostic and monitoring measures and treatment options.
- Hyperthyroidism and hypothyroidism can both lead to heart disease, and thus to increased mortality.
- Hyperthyroidism is associated with tachycardia, raised systolic blood pressure, arrhythmia and atrial fibrillation, mitral valve prolapse and cardiac failure.
- Hypothyroidism is associated with bradycardia, dyslipidaemia and ischaemic heart disease, and contributes to cardiac failure.
- Amiodarone, an important antiarrhythmic drug, can cause hyperthyroidism and hypothyroidism. Amiodarone-induced hyperthyroidism can be especially challenging to treat.
- Careful monitoring of clinical thyroid status, thyroid hormone levels and heart function will guide treatment of these conditions.
- Nonthyroidal illness can alter in vitro thyroid function tests and presents a diagnostic challenge versus thyroid disease, particularly in severe heart illness.
Hyperthyroidism has a prevalence of 1.3% in the general population (0.5% overt, 0.8% subclinical) with an incidence of 0.8 per 1000 women per year, and hypothyroidism has a prevalence of 4.6% (0.3% overt, 4.3% subclinical) with an incidence of 3.5 per 1000 women per year.1,2 Thyroid dysfunction is more common in women (hyperthyroidism 6:1) due to the preponderance of autoimmunity in women. More than 10% of the adult population have circulating thyroid autoantibodies.3
Insufficient or excessive thyroid hormone levels can affect cardiovascular health, either by causing heart disease directly or by worsening existing cardiovascular disease. This article discusses the mechanisms by which thyroid disease can affect the cardiovascular system, the diagnostic and monitoring measures that should be taken for these patients, and treatment options.
Pathophysiology
Thyroid hormones have clear physiological effects on the heart and cardiovascular system. Thyroid hormone excess and deficiency have pathophysiological effects generally similar to, but more extreme than, the physiological effects. The predominant action of thyroid hormones is via nuclear receptors on specific genes with thyroid hormone response elements in their upstream regulatory sequences. These genes include those for cardiac myosin heavy chain alpha, sarcoplasmic reticulum calcium ATPase, sodium-potassium ATPase, atrial natriuretic peptide and voltage-gated potassium channels. Cardiac angiogenesis is increased. Nongenomic actions can influence sinoatrial node activity, transport of calcium, sodium and glucose in myocytes, and possibly oxidative phosphorylation in mitochondria.
Thyroid hormones influence cardiovascular haemodynamics by increasing the force and speed of systolic contraction, increasing heart rate, increasing cardiac output, decreasing systemic vascular resistance, increasing systolic blood pressure and decreasing diastolic blood pressure. Thyroid hormones increase both hypercapnic and hypoxic drives.
All usual forms of hyperthyroidism are associated with suppression of thyroid stimulating hormone (TSH) and elevation of both free thyroxine (fT4) and free tri-iodothyronine (fT3) levels, or fT3 alone (T3 toxicosis). Standard in vitro thyroid function tests are diagnostically reliable, but clinical assessment is paramount in judging severity. Primary hypothyroidism is the most common form of hypothyroidism and TSH levels are elevated even when T4 and T3 levels remain within the normal range (subclinical hypothyroidism); TSH is, therefore, a sensitive index for this diagnosis. In hypothyroidism due to pituitary disease, TSH levels are normal or low; a low T4 level, therefore, is the best in vitro diagnostic marker. Mild pituitary hypothyroidism, however, may not be diagnostically obvious on thyroid function tests and tests need to be interpreted in clinical context, especially as severe nonthyroidal illness can cause apparently similar changes.
Hyperthyroidism
Overt hyperthyroidism is associated with tachycardia, raised systolic blood pressure and widened pulse pressure. Hyperthyroidism can cause angina in patients with ischaemic heart disease, and myocardial infarction in the absence of ischaemic heart disease is described. The effect on respiratory drive can produce dyspnoea in the absence of cardiac failure. Hyperthyroidism is associated with increased all-cause and cardiovascular mortality.4,5 Treatment causing hypothyroidism appears more effective in reducing mortality than therapy producing only euthyroidism.6,7 This suggests that aggressive therapy to control hyperthyroidism, accepting the risk of possible hypothyroidism requiring levothyroxine therapy, may be warranted in patients with hyperthyroidism, at least in the elderly.
Arrhythmia and atrial fibrillation
Palpitations often occur in patients with hyperthyroidism and are usually due to sinus tachycardia but arrhythmia is a common complication. Hyperthyroidism increases the risk of atrial fibrillation; however, ventricular arrhythmias are rarely due to hyperthyroidism. Atrial fibrillation resulting from hyperthyroidism increases the risk of pulmonary embolism and congestive cardiac failure. High normal fT4 levels and low-normal serum TSH levels have been reported to be associated with a modest increase in the risk of atrial fibrillation.8
Anticoagulation in thyroid disease
Both overt and subclinical hyperthyroidism are procoagulant states.9 There are limited data to guide decision-making on the use of anticoagulation in patients with atrial fibrillation. Validated scores such as the CHA2DS2-VASc score can be used with the understanding that exclusive use of these scores may underestimate the risk of thromboembolism in patients with hyperthyroidism. Cessation of anticoagulation can be considered in patients who revert to sinus rhythm after treatment of the underlying thyroid disorder. The efficacy of novel oral anticoagulants (NOACs) in people with atrial fibrillation due to hyperthyroidism is not well studied. Furthermore, their potency may increase as hyperthyroidism comes under control, similar to warfarin.10 However, routine tests for the effects of NOACs are not routinely available, unlike for warfarin, therefore we suggest that warfarin should be currently preferred.11
Use of iodinated contrast media in coronary angiograms on thyroid function
The iodine load in iodinated contrast media can induce hyperthyroidism. The presence of thyroid nodules, older age and a family history of thyroid disease are important positive-predictive factors for iodine-induced hyperthyroidism.12 Evaluation of thyroid function at baseline and three to four weeks post-injection should be considered in patients with these risk factors. Although not routinely recommended, pretreatment with low-dose thionamide before iodinated contrast media administration, and brief continuation for one to two weeks, is a preventive option in high-risk patients (e.g. older, presence of multinodular goitre with autonomy).13
Cardiac failure
Contrary to the physiological effects of thyroid hormones, decreased cardiac contractility is observed in hyperthyroidism, with accelerated apoptosis of myocytes. Cardiac failure can occur solely due to hyperthyroidism, but is more common in association with other cardiac disease. Rate-dependent cardiac failure can occur, with decrease of both left ventricular ejection fraction and diastolic compliance; this can respond to beta blockers. Pulmonary hypertension from hyperthyroidism as a cause of right-sided heart failure has been reported. Hyperthyroidism increases resistance to digoxin therapy. Takotsubo cardiomyopathy has been described in patients with thyroid storm. Although effects of thyroid hormones resemble those of catecholamines, serum levels of catecholamine are reduced in patients with hyperthyroidism.
Amiodarone-induced hyperthyroidism
Amiodarone causes two types of hyperthyroidism (but mixed forms also occur). Type 1 amiodarone-induced hyperthyroidism (AIT) is due to the liberation of inorganic iodine from amiodarone, which contains 37.2% iodine by weight. This type of iodine-induced hyperthyroidism most commonly occurs in patients with pre-existing goitre. Type 2 AIT is due to the toxic effect of organic iodine-containing amiodarone metabolites, causing thyroiditis even with a previously normal thyroid. This generally does not develop before 12 to 24 months of therapy and can occur up to 18 months after cessation of long-term amiodarone treatment.
Thyroid function tests can be diagnostically confusing for a month or so after commencing amiodarone due to the alteration of T4 to T3 conversion in tissues, including the pituitary gland, with distortion of feedback mechanisms. Chronic inhibition of T4 to T3 conversion in the liver, kidney, skin and muscle can result in a raised fT4 level with normal fT3 and normal TSH levels, but this is not hyperthyroidism or a risk factor for hyperthyroidism.
True AIT is characterised by (usually marked) elevation of fT4 and fT3 levels with suppressed TSH levels. Weight loss, proximal myopathy and worsening arrhythmia should provoke suspicion of AIT, and thyroid function tests should be performed routinely every six months. Colour-flow Doppler ultrasound of the thyroid is the most discriminant test to guide therapy as it shows very low flow in type 2 AIT.14
Type 2 AIT is the more common form in Australia, and will usually respond to high-dose prednisolone (40 mg daily for two to four weeks, then reducing). If amiodarone is judged important to prevent ventricular arrhythmia, it need not be stopped in patients with type 2 AIT and does not materially affect response to prednisolone therapy of AIT.14-16
Type 1 AIT may respond to high-dose thionamide therapy. Thyroidectomy may be required in patients with type 1 or 2 AIT if there is no response to pharmacotherapy. Radioiodine therapy is rarely possible in AIT, particularly in type 2 AIT, because of the absence of iodine uptake. However, it may be considered many months later as prophylaxis against recurrent AIT if amiodarone must be resumed. There is no consensus on this approach as the absolute risk of recurrence after resumption of amiodarone is unknown.
Although dronedarone, an alternative noniodine-containing antiarrhythmic agent, does not have the thyroidal or pulmonary side effects of amiodarone, it appears to increase all-cause mortality and heart failure in patients with chronic atrial fibrillation and may have significant hepatotoxicity. Therefore, it seems unlikely to replace amiodarone for treatment of atrial or ventricular arrhythmias.17
Hyperthyroidism and mitral valve prolapse
An association between hyperthyroidism and an increased incidence of mitral valve prolapse in adults and children beyond that seen in the general population has been described. An association of mitral valve prolapse with the autoimmunity of Graves’ disease and Hashimoto’s thyroiditis independent of the hyperthyroid state has been suggested in some studies18 and mitral valve prolapse has been reported in patients with hyperthyroidism and autonomously functioning thyroid nodules.19
Subclinical hyperthyroidism
Subclinical hyperthyroidism is defined as a chronically suppressed TSH level with normal fT4 and fT3 levels. There is a clear increased risk of atrial fibrillation if TSH levels are below 0.10 mU/L.20 In patients over the age of 60 years there may be an increased all-cause and cardiovascular mortality, at least over five years, although this has not been confirmed in all meta-analyses and no interventional data are available.21-23 Additional studies have suggested a relative risk of 2.54 for atrial fibrillation, which is a 3.2% risk increase over 8.8 years if TSH level is below 0.10 mU/L, and a relative risk of 1.63 or a 1.6% increase over 8.8 years if TSH is low but above 0.10 mU/L.24
Hypothyroidism
The haemodynamic effects of overt hypothyroidism are the reverse of hyperthyroidism, with increased systemic vascular resistance, decreased cardiac contractility and decreased cardiac output. Severe hypothyroidism is associated with bradycardia and torsade de pointes; the latter can respond to levothyroxine therapy. Ischaemic heart disease is increased in patients with hypothyroidism,25 especially in those with concomitant hypertension. In animal studies, acute myocardial infarction causes more myocardial damage in the presence of hypothyroidism.26 Myocardial oxygen consumption is decreased in patients with hypothyroidism; this is thought to explain the low incidence of angina. The dyslipidaemia of hypothyroidism contributes to accelerated atherosclerosis. Congestive cardiac failure can occur, but is not common solely due to hypothyroidism. Pericardial effusion is common, but rarely produces tamponade. ECG shows low voltages and ST-T wave changes.
Subclinical hypothyroidism
Subclinical hypothyroidism, in which the fT4 level is within the normal range but the TSH level is elevated, is common and is associated with measurable cardiovascular effects of decreased left ventricular diastolic function, slowed myocardial relaxation, decreased ventricular filling, increased systemic vascular resistance, subtle dyslipidaemia, and decreased endothelial function. Some, but not all, epidemiological analyses report an adverse effect of subclinical hypothyroidism on coronary heart disease events and mortality.27 There is no conclusive demonstration of clinical benefit of levothyroxine therapy in subclinical hypothyroidism; however, the current consensus is that treatment of asymptomatic subclinical hypothyroidism should occur when the TSH level is greater than 10 mU/L.28 Care should be taken to avoid overtreatment of subclinical hypothyroidism with induction of iatrogenic subclinical hyperthyroidism, as data for the increased risk of harm from subclinical hyperthyroidism are stronger than the data for potential benefit from treatment of subclinical hypothyroidism, at least in patients over 60 years of age.29
Amiodarone-induced hypothyroidism
Amiodarone-induced hypothyroidism is more likely to occur if thyroid function is already impaired, and is due to the effect of excess inorganic iodine on the thyroid. As thyroid autoimmunity is the most common pre-existing disease, pretreatment thyroid function tests and antithyroid antibody testing should be performed, and testing continued every six months while taking amiodarone therapy. In general, thyroid hormone replacement therapy is straightforward unless severe coronary artery disease and exacerbation of angina occurs. Replacement therapy with levothyroxine in the presence of ischaemic heart disease should begin at a dosage of 25 mcg daily, and repeat thyroid function tests at not less than four-weekly intervals.
Hypothyroidism and cardiac surgery
Occasionally, overt hypothyroidism and severe coronary disease coexist and thyroid hormone replacement therapy is rendered impossible because it induces angina. In this circumstance, coronary artery surgery can proceed but with strict attention to adjustment of the doses of drugs, anaesthetic agents and fluid replacement required by the markedly reduced drug clearance and hypometabolism of hypothyroidism.
Nonthyroidal illness
Nonthyroidal illness commonly causes the low T3 syndrome. When severe, both T4 and T3 levels are low, without TSH elevation except during recovery. In general, this is thought to be an appropriate response to acute illness that may become maladaptive when prolonged. Limited trials of T4 and T3 therapy in critical illness in animal models or in humans have not shown benefit on mortality.30 The suppressive effect of thyroid hormone therapy on TSH may compromise normal recovery from the low T4 syndrome and promote excessive catabolism.
Thyroid hormone therapy and cardiac surgery including cardiac transplantation
T3 therapy has become part of routine preparation of the donor heart before transplantation because the nonthyroidal illness (lowT3 syndrome) has been hypothesised to be hypothyroidism. The extensive literature on the use of T3 therapy in brain-dead heart donors to improve post-transplant myocardial function, although strongly advocated by some, remains inconclusive.31 Some studies show an apparent benefit, but the interpretation of these findings is confounded by suboptimal experimental design and by other interventions such as insulin, glucose, cortisol and vasopressin.32
Use of pharmacological T3 therapy after coronary artery bypass grafting can increase cardiac output acutely and may decrease the risk of acute atrial fibrillation. T3, however, appears to function mainly as a vasodilator, and there is no beneficial effect on mortality.33,34
Thyroid hormone resistance
Thyroid hormone resistance (RTH) is rare (about one in 40,000 for each form). Two forms of thyroid hormone nuclear receptor mutation have been defined (RTH-alpha and RTH-beta). Autosomal mutations of the thyroid hormone nuclear receptor-beta were the first to be recognised. There is differential tissue expression resulting in variable cardiovascular manifestations in different kindreds but tachycardia is present in about one-half, atrial fibrillation can develop and cardiomyopathy has been described. Abnormal myocardial relaxation and increased systemic vascular resistance are present.35 RTH-alpha is associated with low heart rate and systemic blood pressure unresponsive to thyroid hormone therapy.36 So far thyroid hormone transporter and selenoprotein mutations causing resistance have not been associated with specific cardiovascular abnormalities.
Research
Thyroid hormone analogues have been tested with the aim of benefit on cardiac failure and dyslipidaemia but without the adverse metabolic effects of thyroid hormones. The thyroid hormone analogue diiodo-thyropropionic acid (DITPA) increases cardiac output and decreases systemic vascular resistance in cardiac failure, but has not been shown to produce symptomatic benefit. D-T4 was used to decrease cholesterol levels before other agents became available, but was eventually shown to have no differential benefit on lipid versus adverse thyroid hormonal effects. The trial of DITPA in congestive cardiac failure decreased LDL-cholesterol levels without affecting HDL-cholesterol levels, but increased bone turnover adversely.37
In patients with hypercholesterolaemia, the liver-selective thyromimetic eprotirome has been shown to decrease serum levels of atherogenic lipoproteins without signs of extra-hepatic side effects38 but the use of thyromimetics for the treatment of dyslipidaemia is not currently recommended.39
Conclusion
Hyperthyroidism and hypothyroidism are common endocrine conditions that can seriously affect cardiovascular health. Management of these conditions involves careful assessment of clinical thyroid and cardiac status as well as monitoring of thyroid hormone levels. Choice of pharmaceutical or surgical treatments for thyroid disease and coexistent cardiac disease or cardiac disease and
coexistent thyroid disease must consider the efficacy and safety of potential treatments on both conditions. ET